6th Seminar Report :
The main points to consider when preparing a clinical trial protocol ~From the viewpoint of review process as a medical doctor ~
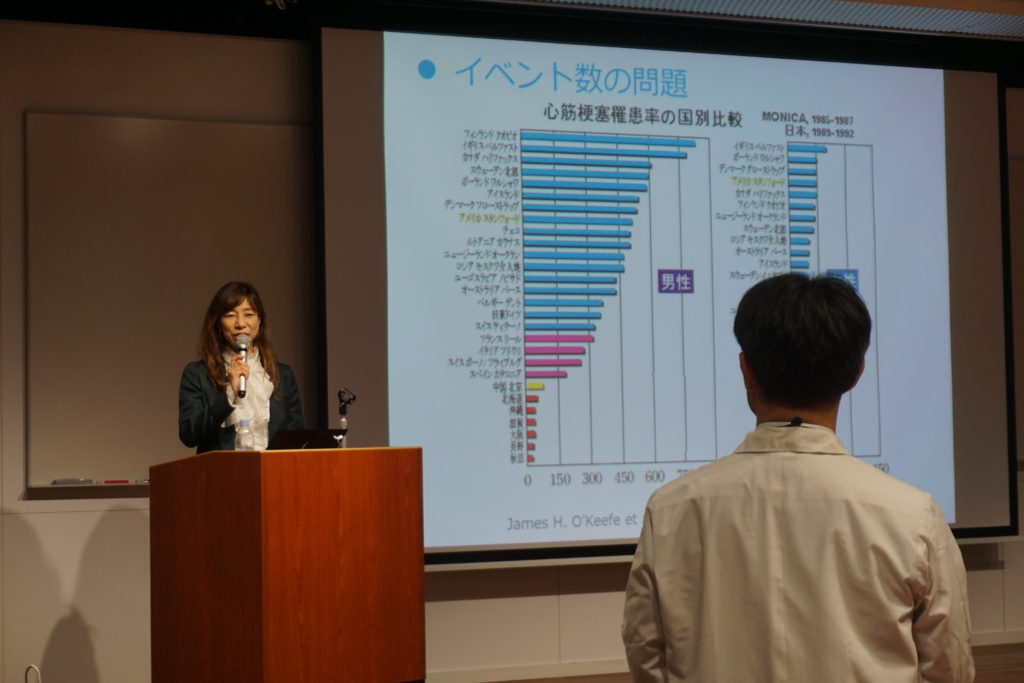
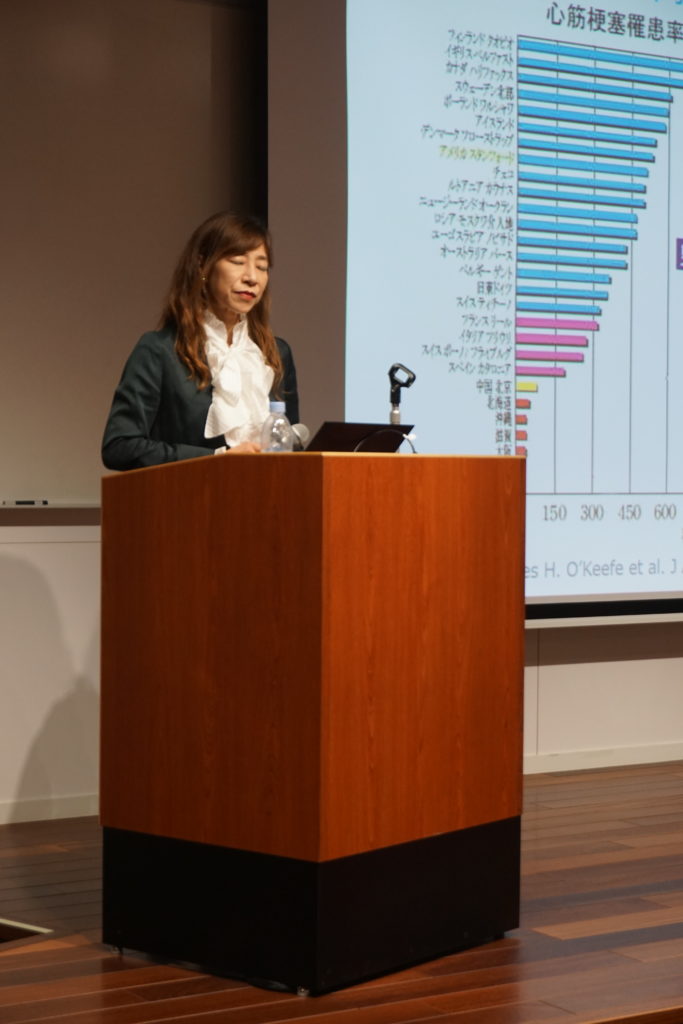
We conducted 6th Academia Research Development Seminar that was the last seminar in 2018FY at Multi Media Hall, Osaka University Hospital on Friday, February 15th, inviting Dr. Kaori SHINAGARA who is from Office of New DrugⅡ, Pharmaceuticals and Medical Device Agency (PMDA). After graduating from the medical school in Japan, she experienced studying in Montreal, Canada. Then she started her carrier at PMDA from 2005, being in charge of clinical trial consultation named “face to face advice” as well as reviewing new drug application from pharmaceutical companies. Her major is arrhythmic field in cardiovascular medicine and she has been deeply dealing with ICH-E14, especially in a part of prolongation of QT/QTc interval that potentially cause fatal arrhythmia.

At the beginning of the lecture, she introduced an organization of PMDA and the basic concept in reviewing new drug application. The main topic of the lecture was important points when preparing an investigator initiated clinical trials’ protocol that are developed by academia. She talked about it from the view point of review process by her experience as a medical doctor. Compared to other countries, basic research is thought to be superior in Japan. In order to proceed research and development for new drugs to get over “death valley”, she introduced “Sakigake Designation Scheme” that is a system to put into practice innovative medicines, medical devices and regenerative medicines initially developed by Japan. It is important for Academia to consult projects as early as possible to PMDA, as clinical trial consultations, she emphasized. The number of consultation such as pre-consultations and face to face advice in 2017FY was over 500. Among those, the number of face to face advice was over 100, she said.
In order to get regulatory approval, PMDA generally assesses not only quality of the data, but also balance between efficacy and safety. Following are essential when new drugs get approval; 1) Reliability of the documents, 2) Superiority of efficacy over safety under appropriate clinical trial design, 3) clinical significance, 4) No risk that are unacceptable over benefit, 5) Quality assurance and supply drugs constantly, she described. In general, more than 2 clinical trials with randomized controlled design are required in order to prove reproducibility of the efficacy for the new drugs that can lead to demonstrate reliability of the data. Furthermore, the review is done with a consideration for assessing a balance between risk and benefit from the view point of disease, characteristics of patients, and clinical significance of the new drug. Unmet medical needs (including superiority of the new drug over standard treatment) and fatal disease or not are also considered in the review process, she explained.

Therefore, investigators need to carefully set; 1) validity of target population, 2) rationale of drug doses, 3) method for efficacy endpoint, when developing clinical trial protocol, she said. We understood what she would like to say was that target population fulfilling inclusion and exclusion criteria must be representative of the disease that investigators focus on, and true endpoint related to clinical significance need to be set especially when pivotal trial is conducted.
In phase II clinical trials (dose finding study), surrogate endpoints may be occasionally used. Notably, investigators need to set surrogate endpoint in relation to true endpoint that will be set in phase III trial. Otherwise, critical issues could occur, she emphasized. Indeed she introduced case examples taken place outside of Japan that clinical trials were conducted with inappropriate surrogate endpoint that was not related to true endpoint. To date, there are only 2 surrogate endpoints that have been established in cardiovascular area including LDL-cholesterol for statin (HMG-CoA) and blood pressure for hypertension, meaning that there are few surrogate endpoints when we conduct pivotal clinical trial, she explained.
In this context, she recommended that investigators need to set secondary endpoint as many as and as wide as possible when conducting exploratory trials that academia mainly focus on. Furthermore, she pointed out more in detail when academia try to perform clinical trials with small sample size for rare disease that 1) to clarify the objectives, 2) necessity of placebo group (not recommended using cross-over design), 3) to avoid difference in baseline demographics, and 4) dose response (because we can’t determine whether insufficient dose or no efficacy, if not obtaining positive results)
After her talk, quite a lot of questions came from audience. Someone asked how we develop new surrogate endpoints. Another asked how we use surrogate endpoints in order to make clinical trial compact. She answered and summarized again that in general, we need to set true endpoint in the pivotal trial and set various kind of secondary endpoints in expiratory trials that academia mainly deal with, in addition to their answer. She kindly and politely responded other questions from audiences. The seminar was ended with huge clap.


We look forward to welcoming more people who are related to research and development, as we would plan to continue the Academia Research Development Seminar in the next fiscal year, 2019.